Control of massive bleeding is all about achieving occlusion of the artery. This is the most important skill we can master as combat medics. Hemorrhaging is the leading cause of death on the battlefield, so we shouldn’t focus on airway, respirations, needle decompressions or other “sexy” interventions until we absolutely have “M” in MARCH mastered.
We stop arterial blood flow by using our hands as a stopgap to buy time for commercial or improvised extremity tourniquets or Junctional tourniquets. These must be placed appropriately and tightened until bleeding stops. But how do we replicate achieving occlusion in training?

A.) Subclavian for injuries where brachial pressure wont work

B.) Example of femoral proximal pressure to but time for Junctional TQ, wound packing or incase both don’t work.
If we are not checking to see if the patients pulse stopped, then we are just LARPing hemorrhage control.
I highly recommend the use of a vascular (not fetal) or if your unit has an ultrasound you can also visualize. Dopplers have been used in emergency departments and OB wards for decades. They are available for your unit to purchase as little as $50+ dollars depending on where you shop, such as Amazon. Dopplers will allow you to listen for the “whoosh” of blood in an artery every beat. More importantly, they will let you know when the blood stops. The same can be done visually using an ultrasound doppler with color-motion enabled, but it can be cumbersome to use during training and every unit may not have an Ultrasound due to cost.
(Credit to @CTOMS Instagram showing a Doppler on radial artery for a TQ application)
Doppler will make your hemorrhage control classes more authentic and consistent, as well as confidence building. There is no “eyeballing” that your junctional tourniquet is tight enough or the student waiting for the instructor to tell them it’s alright. You hear it or you don’t. The tourniquet is working or it’s not. Your indirect or proximal pressure is in the wrong place or it’s dead on. Sometimes it’s just a few centimeters off. You will quickly learn that your entire body weight just 1 inch away from an artery is useless compared to accurate fingertips in the correct area. You want to be a hemorrhage control sniper.
Every medic should be able to stop the blood flow to an arm or leg using subclavian or femoral pressure with their hands, in under 30 seconds.
Every medic should be able to apply a TQ under 30 seconds. A commercial or improvised Junctional TQ under 90, preferably under 60 seconds. Junctional TQs should also be practiced being applied while someone else is holding proximal pressure with their fingers. 90+ seconds is a long time to wait while messing with a junctional, especially improvised. Stop bleeding now and buy time to work towards hands free. If you are unable to get hands free due to severity of injuries, you at least have your hands to fall back on.
 ( Credit to @pog_photography on Instagram )
( Credit to @pog_photography on Instagram )
See for yourself how long it takes you to get junctional tourniquets to work, such as the Croc, SAM or JETT, or even a knee in the abdomen or hand over femoral artery. Try this on radial artery and posterior tibial artery. Hold medics to a standard and let them gain the confidence of turning off a human artery, as close as you can get without actually cutting it with a scalpel. (Not recommended.)

“What if I don’t have a cheap doppler or unit doesn’t have an ultrasound?”
If you don’t have this, pulse checks and pulse oximetry may help until you get one, but are not as accurate. Still, they are better than not checking. (I have seen junctional TQ classes where everyone still has their boots on.)
Best: Ultrasound with Doppler flow ($$$$)
Better: Vascular doppler ($$)
Decent: Pulse Ox +/- palpation ( Unit should already have, but they measure capillaries and may turn off before artery does)
Minimum: Palpating pulses. (Free, but if you aren’t checking pulse BEFORE they apply intervention then it may be difficult to tell if you are in right area or it’s just not weak. Weak pulse risks continued hemorrhage and compartment syndrome.)
While a doppler is generally too difficult or time consuming to hold still during a full trauma lane, this is good for training and testing them on just the intervention itself in an air conditioned room before full stress trauma lanes. We don’t want to test them on a trauma lanes on something they cant do in a calm controlled situation first. Once we know they can do it in a calmly controlled environment well, we can use our fingers and pulse ox to assess adequacy during a trauma lanes without slowing it down or taking an administrative pause.
Doppler tips: One issue that comes up is holding the doppler to keep it in the right place so it can still “hear” the artery. I recommend not holding it up high, but hold it like a pencil with your wrist resting near the pulse location to steady your hand so it isn’t floating trying to stay on an artery while medic is manipulating limb applying pressure. You can also use your opposite hand to hold the probe in place in between your fingers. Marking the location with a permanent marker may also help.
Join the Discussion on Instagram:
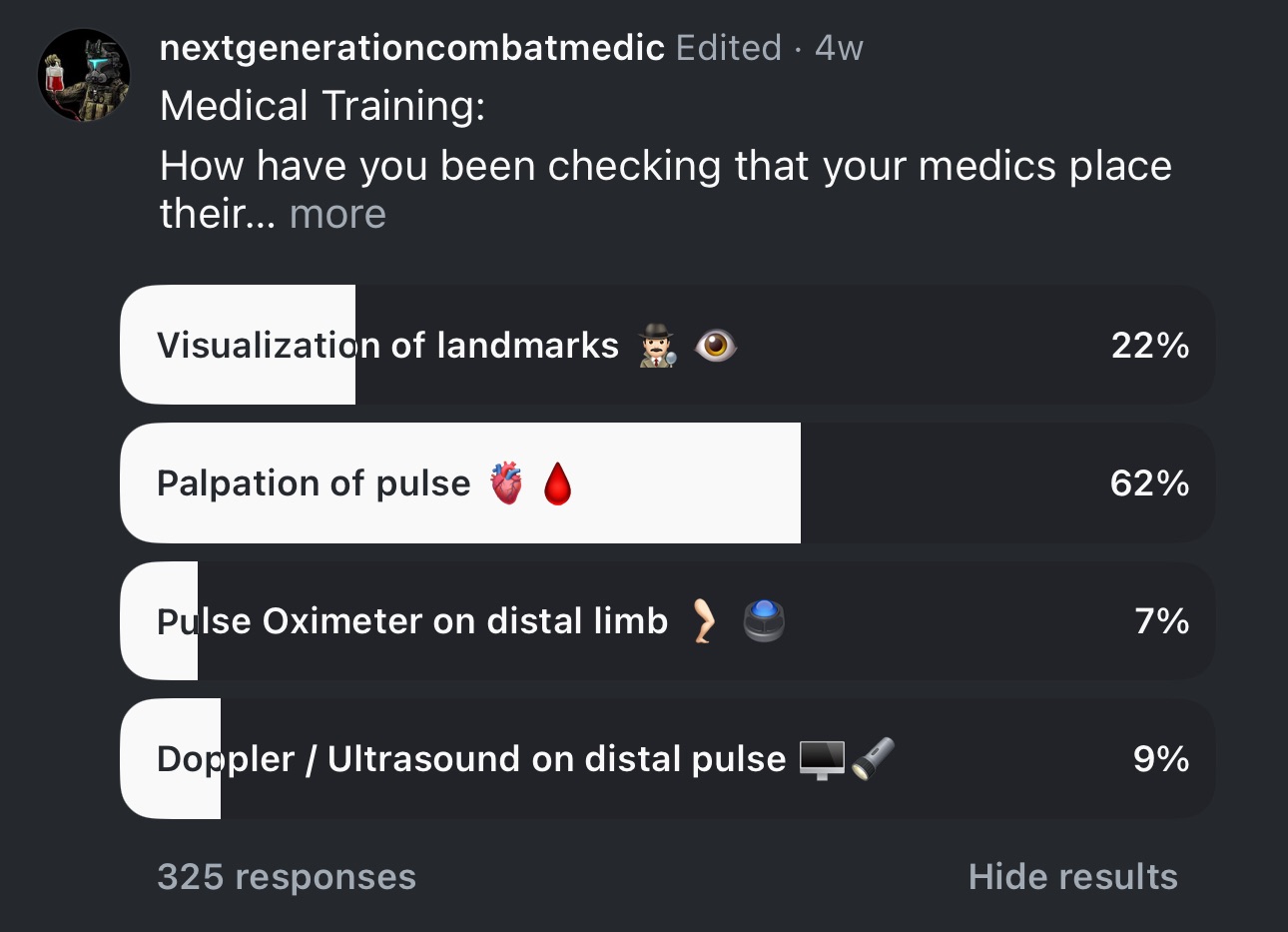
See our post on what other medics are using to teach hemorrhage control.
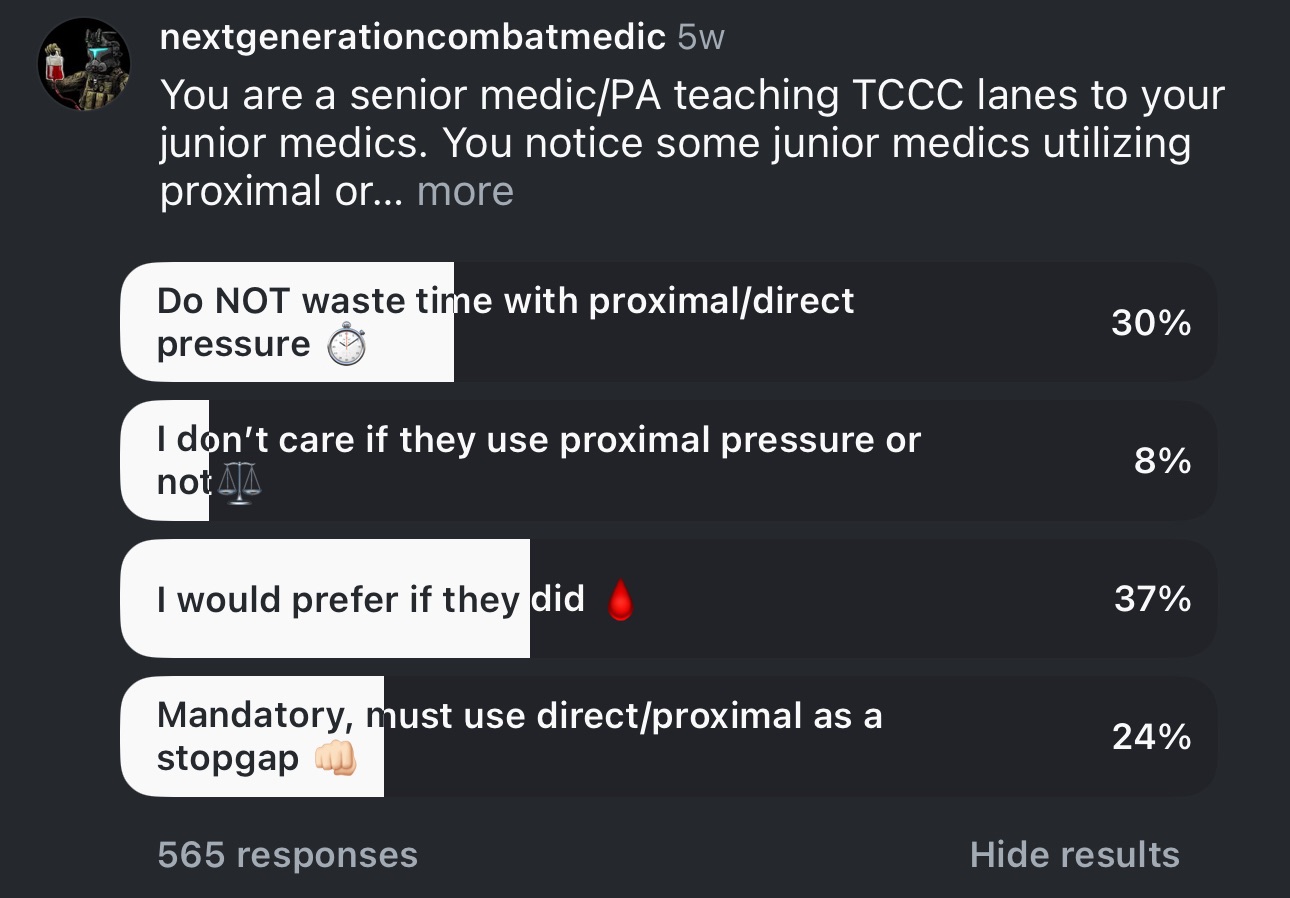
See our post on how much proximal pressure is emphasized during others training.
If you try out this article below, post some of the slowest and fastest times your team had when trying this out!
🐇